The ThinkCancer! Phase III Trial
Introduction
After an overwhelmingly positive reception from participating GP practices during a recent feasibility study, Phase III of ThinkCancer! will be launching in the coming weeks! The study will test the effectiveness of a multi-faceted, intervention which aims to streamline cancer diagnosis in primary care. The intervention utilises a whole practice approach and consists of a series of three unique workshops. The first two are education in nature and are delivered separately to clinical and non-clinical staff. In the third workshops, the entire practice team co-develop their own bespoke safety-netting plan. It is anticipated that this will help to shorten the interval between a patient first presenting to primary care with a symptom suggestive of a possible cancer, to their onwards referral to secondary care for definitive diagnosis and treatment.
During the next phase of the study, we will be recruiting GP practices from across Wales and the North West of England. If you would like to find out more about phase III of ThinkCancer! or are interested to take part in future studies, please email the team at: WICKED@bangor.ac.uk
........................................................................................................................................................................................................................
The Study
The aim of the ThinkCancer! study is to determine the feasibility of a future definitive randomised controlled trial (RCT) of this complex intervention compared with usual primary care. A feasibility study explores whether a future, larger-scale definitive trial can be done. This incorporates testing practice recruitment, the delivery of the intervention and also the outcome measures so that we can refine the intervention as we go along. This will in turn guide the design for a future trial. These are important steps in the development of successful randomised controlled trials and the implementation of their findings into practice.
The ThinkCancer! feasibility study will begin in the autumn of 2019. We will be looking for practice teams to take part in this study to test the intervention. For more information, please contact the study team on wicked@bangor.ac.uk
WICKED (Wales Interventions and Cancer Knowledge about Early Diagnosis)
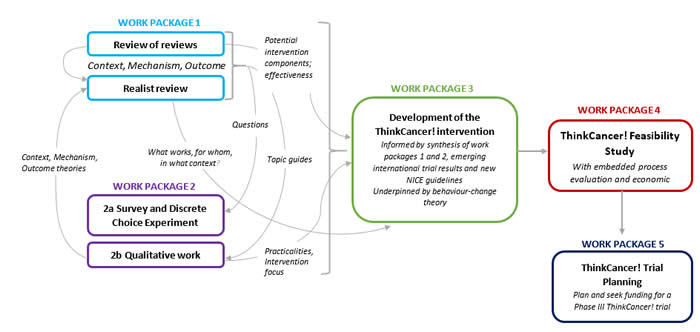
The ThinkCancer! Study comprises Work Package 4 of a programme of research called the Wales Interventions and Cancer Knowledge about Early Diagnosis (WICKED). The overall aims of the WICKED Programme are to improve the quality and consistency of primary care approaches in order to improve timely diagnosis of cancer. Ultimately, this feasibility study will inform Work Package 5, which will encompass the planning phase for a future definitive Phase III Trial.
Work Packages 1 and 2 informed the development of the ThinkCancer! Intervention. We used a variety of methods to collect and integrate data from different sources:
- Comprehensive reviews of published literature, relevant reports and web pages,
- Online survey including a Discrete Choice Experiment (DCE) sent to all GPs in Wales
- Twenty telephone interviews with GPs
- Focus groups held with four practice teams.
A target behaviour – GPs thinking of and acting on clinical presentations* that could be cancer - was agreed on based on the findings from the first two Work Packages.
The work was underpinned by Behaviour Change Theory and informed by stakeholder consultation at every stage. Patients and the public have been and remain involved at all stages of the project.
Read more about the WICKED Programme and the previous Work Packages by clicking here to read our publication in the BJGP.
*clinical presentations: symptoms, clinical signs and the context (e.g. past medical history, risk factors, previous consultations) during a primary care consultation.
Patient and Public Involvement
Janice Rose has worked with us throughout the WICKED programme and is a key member of the ThinkCancer! Team.
‘I got involved with researchers working in the field of cancer after my breast cancer diagnosis and my mum’s diagnosis of Cancer of Unknown Primary (CUP). Both happened in 2009. Since then I have worked locally, regionally and nationally with researchers representing the patient perspective in various research studies taking place and generally helping research into cancer where I can.
My link to the Wales Interventions and Cancer Knowledge about Early Diagnosis (WICKED) Programme came through my link to the NCRI Primary Care Group. I have worked with the researchers since the study started.
I am pleased to be one of the patients working with the research team looking at ways to help doctors and other staff in GP practices in Wales to help improve early cancer diagnosis for their patients. The project is very worthwhile as early diagnosis of cancer is so important for patients in terms of the outcomes after their diagnosis.
Having patients working with the research team allows for the voice of the patient to be listened to and considered throughout the research project. Very important.'
- Janice Rose, ThinkCancer! PPI Representative
This project has been funded by Cancer Research Wales

For more information about this study, please contact the study team on wicked@bangor.ac.uk
© Bangor University




